Dr. Bernard Jankelson introduced the term Neuromuscular Dentistry to the dental profession in 1967. The masticatory system is a three dimensional system composed of Teeth, Temporomandibular Joints and Muscle. Without muscles the masticatory system is static and non-functional. Neuromuscular dentistry is a comprehensive concept of a dynamic masticatory apparatus that follows universal anatomic and physiologic laws.
However, dentists did not have the technology or protocols to objectively evaluate and diagnose masticatory muscle function/dysfunction or predictably restore masticatory muscles to optimum function. Yet, there is universal consensus that 90% of temporomandibular dysfunction is myogenous in origin. The dental profession operated in a two dimensional field of teeth and temporomandibular joints. Qualitative or quantitative evaluation of the important muscle component could not be possible until development of appropriate measurement technologies. Neuromuscular dentistry operates in a dynamic three dimensional field of teeth, joints and muscle.
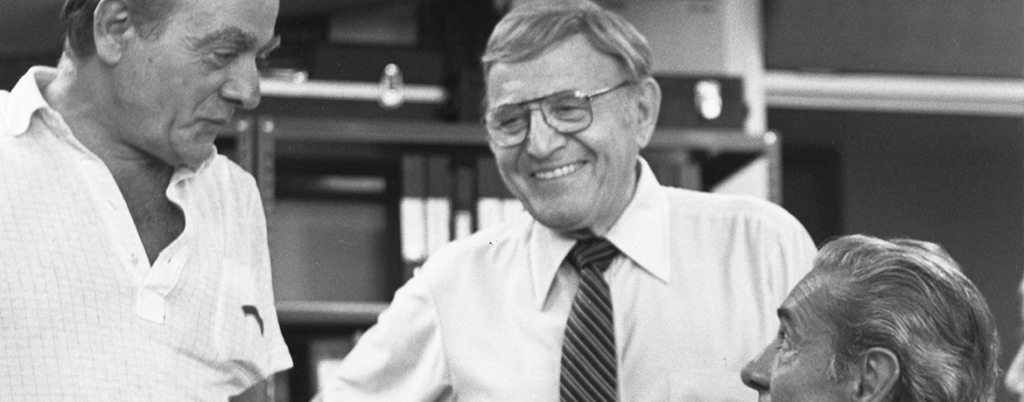
The seed of neuromuscular dentistry begins with a little told story of how Dr. J., as he was known to friends and colleagues, became involved in neuromuscular medical research at the University of Washington and University of Oregon Schools of Medicine. In the early 1940’s his beloved wife, Cherub, developed symptoms of neuromuscular disorder characterized by muscle weakness, vertigo, visual disturbance and other non-specific neuromuscular symptoms. He traveled the world looking for answers and a diagnosis. One of the leading experts on what is now called multiple sclerosis was a physician, Dr. Jonez, at nearby Tacoma St. Joseph Hospital. The diagnosis was made. In the early 1940s there was no known treatment. Dr. Jonez and Dr. Jankelson began a friendship and collaborative search for answers.
Drs. Jonez and Jankelson theorized that the problem was related to degenerative changes in the conductive myelin sheath of the nerves that prevented proper electric conduction. The next hypothesis was based upon the fact that myelin is a prodigious consumer of oxygen. Their early collaboration focused on ways to get more oxygen to the myelin sheath in order to prevent nerve degeneration. Dr. J continued to work with physicians and physiologists at the University of Washington and Oregon Bioengineering Departments following the hypothesis of possible beneficial therapeutic effects from increasing oxygen availability to thwart the continuing nerve degeneration. Something must have worked because his beloved Cherub lived a productive and happy 86 years.
With this early background, the genesis of neuromuscular dentistry began with the collaboration of Dr. Bernard Jankelson and Dr. H.H. Dixon, a renowned muscle physiologist, working together at the University of Oregon School of Medicine in the early 1960’s. The technology to change muscle metabolism and muscle resting states with low frequency TENS was the breakthrough that brought dentistry into a 20th Century paradigm consistent with the rapid technology associated with modern medicine. The electrical parameters established by Dixon and the insight of Jankelson to deliver the stimulus via the coronoid notch to proximate Trigeminal (V) and Facial (VII) cranial nerves exiting the cranium provided, for the first time, the technology whereby the dentist could directly alter the metabolic state of masticatory muscle to facilitate diagnostic and treatment outcome.
Dr. Jankelson assembled a R&D group of former Boeing engineers and biomedical engineers in 1970 to develop biomedical instrumentation to track jaw movement in three dimensions. Four years later, in 1974, the first clinical jaw tracking device was introduced. The system sensed the location of a small magnet attached to the labial of the lower incisor teeth helping the clinician diagnose and treat occlusal mandibular dysfunction with objective physiologic measurement data.
Technology to monitor masticatory muscle activity at rest and in function in a clinical environment was necessary to elevate diagnosis and treatment of occlusion from art to science. Surface electromyography (sEMG) is the technique by which the action potentials from muscle fibers are recorded and displayed. This technology became available to the dental clinician in 1979. Real time sEMG was integrated into the three dimensional computerized jaw tracking system in 1987, allowing clinicians to objectively correlate muscle activity and jaw position.
Because of the creative insight and perseverance of Dr. Bernard Jankelson, neuromuscular principles and techniques combined with state of the art technology applying universal anatomic and physiologic principles help trained clinicians treat patients with temporomandibular disorders, complex restorative problems, restoration of edentulous patients and orthodontic treatment. The management of occlusion as a dynamic three dimensional biologic system, rather than a static two dimensional system, allows the trained neuromuscular dental clinician to diagnose and manage difficult occlusal problems with predictable outcome never before attainable.
Historically, TMD’s were referred to as TMJ or TMJD when the disorder was considered only to involve the temporomandibular joints. Currently, the name TMD is used to describe a group of diseases that can involve the jaw joints, the muscles that control jaw movement and the dental occlusion. They are physical/functional disorders arising from an imbalance in the delicate working relationship of the jaw and skull with the muscles that move the jaw and the nervous system associated with them. This imbalance results in muscle fatigue, spasm and/or joint dysfunction, and even changes in the form and position of the teeth, which in turn cause a variety of symptoms.
In order to understand what appears in some patients to be global manifestations of TMD, we must understand that the complex stomatognathic system is comprised of the central nervous system in conjunction with the dentition, masticatory muscles and temporomandibular jaw joints all functioning in harmony with one another and its interconnections with the entire musculoskeletal system. Everything is connected and dysfunction in one part can affect dysfunction in other parts. In contradistinction, healthy function in all parts of the stomatognathic system along with proper cranio-cervical posture and healthy airway contribute to homeostasis.
Various concepts of dental occlusion are used in dentistry today. Members of ICCMO have adopted the neuromuscular occlusion philosophy. This physiological approach is based on the creation of dental occlusion position synchronized with relaxed balanced masticatory muscle function. How this is achieved and how neuromuscular occlusion is applied in various fields of dental practice including complex restorative dentistry and orthodontics that will be described in this website.
For patients suffering from various manifestations of TMD, neuromuscular dentistry has allowed clinicians the opportunity to help a growing number of patients that were unable to obtain alleviation of their clinical problems previously by dentists and other health care providers.
The study of neuromuscular dentistry allows the clinician to understand orthopedic principles and dynamic physiologic occlusion concepts more comprehensively than traditional static dental paradigms. Computerized measurement devices record and permit analysis of mandibular movements, dental occlusion, masticatory muscle function and TMJ joint sounds provide objective information to help dentists treat patients successfully, rather than only relying on subjective symptoms reports from patients and clinical observations throughout treatment.
The recognition of musculoskeletal clinical signs including occlusal flags and subjective patient symptoms aid in the establishment of an accurate diagnosis of acute and chronic pain patients as well as patients requiring the establishment of a new dental occlusion. In the initial stabilization phase of TMD therapy through the creation of a physiological therapeutic neuromuscular occlusion, it is necessary to identify an optimal starting point of physiologic rest and then select a therapeutic stable occlusal position. This phase of treatment utilizes a fixed or removable oral orthotic appliance.
Removing all afferent and efferent noxious proprioceptive stimuli of occlusion and objectively measuring all muscle and postural responses of the mandible will allow the dentist to remove harmful muscle torques and strains that relate to the health or dysfunction of the trigeminal system.
In summary, the importance of a physiologic occlusion cannot be over-emphasized in treating TMD patients.